Which sequence correctly describes the three phases of hypothermia during general anaesthesia in infants? - Answer & Explanation
- Non shivering thermogenesis → Redistribution → Shivering thermogenesis
- Redistribution → Thermal imbalance → Thermal steady state ✓ Correct Answer
- Shivering thermogenesis→ Redistribution → Rewarming
- Thermal imbalance → Redistribution → Thermal steady state
Explanation:
Phases of Hypothermia Under Anaesthesia
Hypothermia under anaesthesia progresses through three characteristic phases.
Phase I: Internal Redistribution [30-60 minutes]
The first phase occurs immediately after induction of anaesthesia and is characterised by a rapid decrease in core temperature. This decline results from anaesthetic-induced vasodilation, which expands the core, spreading the heat over a larger volume, allowing warm core blood to flow into cooler peripheral tissues. Importantly, total body heat content does not change significantly during this phase; rather, heat is redistributed within the body.
In infants, redistribution hypothermia is particularly pronounced because of a relatively small core compartment and rapid equilibration between core and peripheral tissues.
Phase II: Thermal Imbalance [2-3 hours]
Following redistribution, core temperature declines in a more gradual, linear fashion. This phase reflects ongoing heat loss exceeding heat production. Infants lose heat faster than adults during this phase
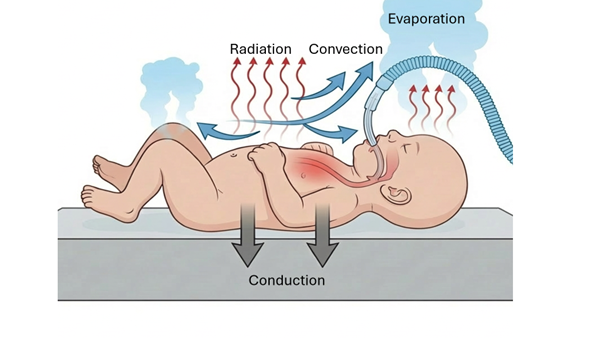
Mechanisms of heat loss
Radiation to cooler surroundings,
Convection from air movement,
Conduction to cold surfaces,
Evaporation from exposed skin, surgical sites and respiratory tract
Reduced heat production under Anaesthesia
Reduced metabolism
Reduced muscle activity and usage of neuromuscular blocking drugs
Reduced work of breathing
Phase III: Plateau/Rewarming/Thermal Steady state
Continued cooling eventually triggers thermoregulatory vasoconstriction. Significant vasoconstriction within the central and peripheral compartment shrinks the size of the core. The peripheral compartment also behaves as a buffer between the low environmental temperature and the core.
The metabolic heat produced is restricted to the smaller central compartment enabling the core temperature to stabilise or even increase gradually.`